Modeling the Future of Medical Devices
“We’re here for the patients we serve. We’re here to make health care better.”
That’s how Walter Schmidt, senior manager of the modeling and simulation team at Stryker Orthopaedics, puts medical device testing and standards work in context.
Of the devices themselves, Jeffrey Bischoff, director of biomechanics research for Zimmer Biomet, adds, “We all want to get good devices out, and out quickly. The right standards can help to make this happen.”
With today’s modeling technologies, which push the boundaries of testing medical devices, a faster, more efficient path to the marketplace can be taken. These approaches lead to more durable artificial knees and hips as well as improved vascular stents. Someday, these highly tailored processes will likely be used to design and evaluate a patient-specific prosthetic heart.
Time to Market
“Modeling, if done well, provides a way of understanding performance more comprehensively than benchtop physical testing,” says Bischoff, a member of ASTM International’s committee on medical and surgical materials and devices (F04).
FOR YOU: The Future of Exoskeleton Standards
Computational modeling, in which a computer simulation is used to study fatigue, fracture, and other aspects of a system, offers the opportunity to shorten the time needed to design, build, and test medical devices. With a computer-aided design in hand and a model to run, potential device weaknesses can be identified and addressed earlier in the design process, while potentially successful devices can be verified more quickly than with traditional testing.
Among the forms of computational analysis, finite element analysis (FEA) has long been used to simulate what a device will undergo in actual use. “FEA is used for structural analysis. It enables the evaluation of stresses and strains, so ultimately fatigue life,” says Brian Choules, technical director for BDC Labs and chair of the cardiovascular standards subcommittee (F04.30). “We can alleviate the need for a significant amount of [bench] testing by using computational modeling.”
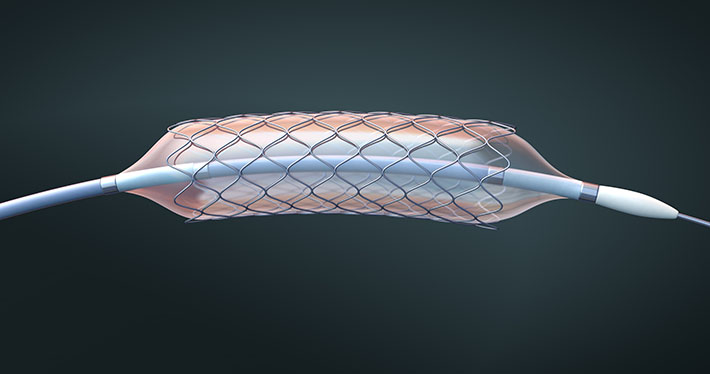
For example, FEA can provide insight on a stent’s ability to perform the hundreds of millions of cycles it would experience in an artery, or the number of times an artificial knee will be able to bend when in actual use.
While the FDA has traditionally relied on three “bodies of evidence” (animal testing, bench testing, and clinical trials) to allow medical devices to be marketed in the United States, the use of computer simulation and computer modeling in support of device approval submissions is increasing.
And for stents and orthopaedic implants, ASTM International standards support FEA modeling.
Square One
ASTM International published its first FEA medical device standard in 2008: the guide for finite element analysis of metallic vascular stents subjected to uniform radial loading (F2514). The F04.30 subcommittee oversees the standard, which notes the value of FEA to evaluate metallic stent performance and to quantify internal stresses and strains.
Schmidt says that when he arrived at Stryker in 2001, the F04 committee had no computational modeling standards. “Regulatory bodies would see regulatory submissions leverage computational simulation to identify the worst-case implant size. However, these computational models would vary widely in terms of components being modeled and modeling assumptions. As such, there was no ability for the regulatory body to internally compare designs between companies. Moreover, it raised questions regarding which simulation model was more suitable,” he says.
To address the situation and as a prelude to the committee’s standards work in this area, F04 held a medical device computational workshop in April 2004. Coming out of the workshop was a new group to address FEA for implants in the arthroplasty subcommittee (F04.22).
The new group began with a proposed general guidance standard. Then, through an interlaboratory study, the group found that assumptions for models varied, as did the analyses. To address the situation, the task group moved toward using a prescriptive, worst-case size selection approach in the standard.
It took time, and in 2013, the practice for FEA of non-modular metallic orthopaedic hip femoral stems (F2996) was approved. The standard establishes the requirements and considerations for FEA analysis to estimate stresses and strains.
Since then, additional orthopaedic FEA standards have been completed:
- Test method for finite element analysis (FEA) of metallic total knee femoral components under closing conditions (F3161), and
- Practice for finite element analysis (FEA) of metallic total knee tibial components (F3334).
And now, recent guidance from the U.S. Food and Drug Administration (FDA) and a recent verification and validation standard (V&V 40) from the American Society of Mechanical Engineers (ASME), which focus on modeling, are also a consideration.

Computational modeling is now an accepted part of the FDA approval process.
As a result, in November 2019, medical device professionals gathered at a workshop, Medical Device Standards Utilizing Computational Modeling, to discuss the FDA guidance, ASME V&V 40, modeling, standards, and the path forward. The F04 groups are looking toward how the FDA guidance and the ASME V&V 40 standard should be considered in ASTM modeling standards.
Part of the Process
The FDA guidance, issued in draft form in 2016, came out in 2018. The document, “Reporting of Computational Modeling Studies in Medical Device Submissions, Guidance for Industry and Food and Drug Administration Staff,” states that “Computational modeling and simulation studies, together with bench, nonclinical in vivo, and clinical studies, can be used to evaluate the safety and effectiveness of medical devices.”
As Bischoff puts it, “The FDA, over the last few years, has become more receptive to modeling. It can be a quicker path to a more comprehensive evaluation of a device, provided the analyst has established the appropriate level of credibility, or confidence, in the accuracy of the model.”
“This document aims to establish uniformity in reporting CM&S [computational modeling and simulation] studies,” as its scope notes. What’s key is information showing that computational studies, which can be FEA or other types (fluid dynamics, electromagnetics and optics, ultrasound, and heat transfer), determine safety and effectiveness.
In addition to its own guidance, FDA has taken a major role in developing the ASME V&V 40 standard published in 2018.
Establishing Credibility
ASME V&V 40 is the standard for assessing credibility of computational modeling through verification and validation: application to medical devices. Industry, medical and research groups, regulators, and academia collaborated on V&V 40, which provides a framework to establish the credibility of a computational model. Schmidt says, “If anyone is going to build a model, they need to follow this recipe to show credibility.”
“It’s a pretty game-changing document in the way it looks at verification and validation of computational models,” adds Choules.
V&V 40 embeds the concepts of context of use, model risk, and credibility to determine whether a computational model is credible for decision making, that is, performs as needed to further a patient’s well-being.
Bischoff summarized the V&V 40 framework at the November 2019 Medical Device Standards Utilizing Computational Modeling workshop with these points:
- “Context of use” defines the role that a computational model has in informing a specific decision on a device, such as a model to determine an implant size with the highest stress, which will then be fatigue tested in the lab and the results compared to a successful device;
- “Model risk” refers to the possibility that the simulation may lead to an incorrect decision that would in turn lead to an adverse outcome; and
- “Model credibility” represents the confidence in the predictive capability of the model for the context of use.
“With the release of the ASME V&V 40 document, it became clear during work on ASTM computational standard practices that the user community was interested in including aspects of the V&V 40 method in current and future ASTM standards,” says Jeffrey Sprague, senior regulatory affairs program manager at Metronic. The workshop helped lay the groundwork for how the group wanted to integrate V&V 40 methodology into ASTM standards.
Seeing an Opportunity
“What we’ve seen in the field is a lot of people really wrestling with how we can effectively utilize the standards that have been out there for years from ASTM while still being cognizant of the need for appropriate model verification and validation that has come out in V&V 40,” says Bischoff. “We needed to bring those two groups [ASME and ASTM International] together.”
Bischoff, Choules, Schmidt, and Sprague, with the sponsorship of the F04 committee, organized and co-chaired the workshop. They agreed on the need to gather interested professionals to discuss the guidance documents and standards and to agree on a path forward for F04 work.
“There’s a great opportunity to do more with modeling and for ASTM, as a standards organization, to help to ensure that it’s done in the best possible way,” Bischoff says. The workshop provided the opportunity to take the next best steps.
About 60 attendees, representing 40 different medical device manufacturers, the FDA, and other constituents, gathered for the day’s sessions (see sidebar). In addition to formal presentations, discussion involved all those present. Attendees strategized that, going forward, modeling should be included in standards, and that modeling standards should have generic models and simulation results, while allowing for company-specific verification and validation evidence.
Sprague feels the most important workshop result is “the strategic roadmap for integration of V&V 40 methodology and terminology into ASTM standards. This will help to increase the rigor and validity of computational methods.” He adds, “We left the workshop with an agreed upon strategy for how the V&V 40 methods and terminology will be integrated into the ASTM standards.”
The Future
With the workshop information, and guidance from FDA and ASME, F04 subcommittees are moving forward with goals in sight.
“There is momentum with our cooperation,” Bischoff says.
And as part of that momentum, Schmidt says, “Industry is looking to this group (F04) to lead computational modeling standards development.”
Workshop organizers anticipate that cooperation from the workshop will be reflected in the upcoming F04 subcommittee efforts and through ongoing conversations among the workshop attendees.
A revision to F2996, the FEA hip femoral stem practice, has begun, and the standard is being updated to reflect the language and sense of V&V 40.
In addition, a proposed practice for spinal fusion cage computational modeling (WK64097) is underway, which will include best practices for FEA for determining the mechanical performance of spinal fusion cages. [Spinal fusion cages use hollow metallic cylinders filled with bone graft that allow vertebrae to fuse together.]
Choules also anticipates more standards related to the loading of test stents (axial and torsional, among others) to reflect the complex nature of the role of stents in the body.
The dream of using modeling to design and evaluate a patient-specific heart may still be in the future, but the promise of modeling methods, and the standards that support modeling, will help make it a reality someday. For now, computational modeling will help many useful medical devices gain approval and help patients sooner.
2019 Workshop on Medical Device Standards Utilizing Computational Modeling
Sessions Included [Full Lineup]:
- ASTM Modeling Standards — Initiation, Evolution, and Current State
- ASME V&V 40 — Philosophy and Practical Considerations
- Applications of V&V 40 to ASTM Modeling Standards — Experiential Learning
- FDA Perspective on Modeling Standards
- Co-Development of Test and Modeling Methods
- Applications of V&V 40 to ASTM Test Standards — Experiential Learning
 SN Home
SN Home Archive
Archive Advertisers
Advertisers Masthead
Masthead RateCard
RateCard Subscribe
Subscribe Email Editor
Email Editor